Monday, June 15, 2020

Two new specimens of Asian giant hornet have turned up in the Pacific Northwest, suggesting that the invasive species made it through the winter despite efforts last year to stamp out the menace to North America’s honeybees.
A big, yellow-and-black insect found dead in a roadway near Custer, Wash., has been identified as the Asian giant hornet, or Vespa mandarinia, Sven Spichiger, an entomologist at the Washington State Department of Agriculture, announced May 29. It was “probably a queen,” he said, from a brood in a 2019 nest and now ready to found a colony of her own.
Canadian scientists have also confirmed their first giant hornet of 2020, a specimen spotted May 15 in Langley, British Columbia.
Dubbed the “murder hornet” to the annoyance of entomologists, the predator earns its nickname from its proclivity to nab a honeybee, bite off the bee’s head carried home to nourish young hornets. Raiding parties of several dozen Asian giant hornets can kill whole hives containing thousands of bees in a few hours.
Those are just some of the details that make V. mandarinia the newsiest stinging invader in years. It’s a fierce little predator, though not as apocalyptic as “murder hornet” headlines have suggested.
Amid the uproar over the “new” hornets, a few facts have been overlooked. For one, North America has previously had at least one close call — not publicized at the time — with the world’s largest hornet. Unlike the current sensational invasion, however, that early episode had a happy ending, at least for the people and native insects of North America. Not so much for the hornets. What’s more, these aren’t the only big, bad hornets that have arrived at the borders of the continent.
Here’s what we know so far, and what we don’t, about Asian giant hornets and the threats they pose.
Is this ‘invasion of the giant hornet’ really new?
Not entirely. What’s new for North America is that last year scientists confirmed Asian giant hornets in the wild.
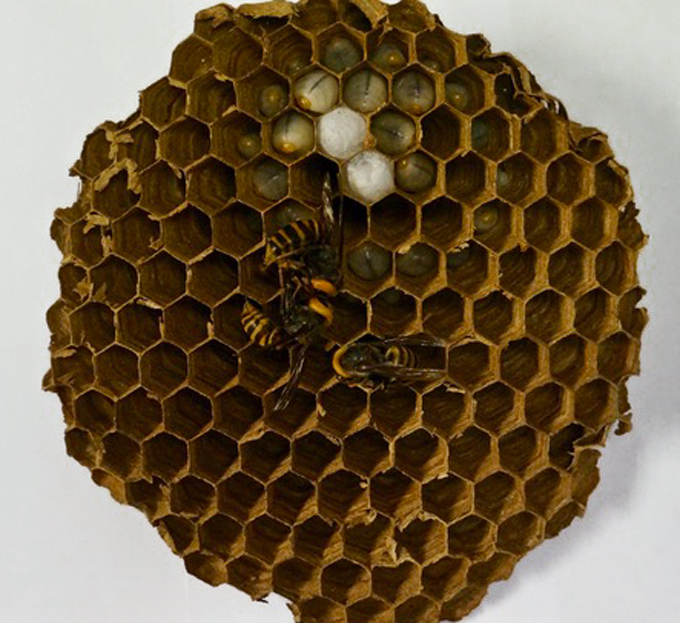
In September 2019, beekeepers tracked down and destroyed a hornet nest about the diameter of a large grapefruit near a public footpath in Nanaimo near Vancouver, Canada. Lone flying hornets also showed up on both sides of the Canada-U.S. border, one at a hummingbird feeder near Blaine, Wash.
But that wasn’t the Asian giant hornet’s first touchdown on North American soil. California had an overlooked close call in 2016. It wasn’t just some lone hornet hiding in a cargo container, says entomologist Allan Smith-Pardo, now at the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service office in Sacramento, Calif. He was the scientist charged with identifying any suspicious wasps or bees found in cargo or mail nationwide. An inspector flagged an express package coming into the San Francisco airport without any mention of insects in its labeling. Yet it held some kind of papery honeycomb-like nest.
Is the Asian giant hornet the first hornet to try invading North America?
Far from it.
The hefty, though not record-setting, hornet V. crabro spread from Europe into New York state around the mid-19th century. Now found in scattered places east of the Rockies, the European hornets nest in hollow trees and cozy nooks within walls. Humans who blunder too close can get painful stings, says Bob Jacobson, a retired entomologist in Cincinnati with a long-standing interest in hornets and venoms. His cousin was stung by the species.
Like the Asian giant hornet, the European invader attacks honeybees, and Jacobson has seen it go after bumblebees, too, as well as yellow jackets and some other wasps. Unlike the new invader, though, a V. crabro hornet hunts alone. It picks off a bee on a flower or at a hive but doesn’t gang up in groups for mass slaughter of whole insect colonies.
Other hornets have also turned up in North America without stirring public interest. That data search of interceptions in California between 2010 and 2018 showed that inspectors stopped four other species besides the giant. In Canada, just in 2019, entomologists identified two different invasive hornet species, including V. soror, which is almost as big as the Asian giant. Whether those arrivals could make a permanent home remains to be seen.
Let’s back up. What are hornets, and why do people get so spooked by them?
True hornets are big, predatory, colony-forming wasps, in the Vespa genus. Apart from the European V. crabro, they’re native to Asia. They need meat to feed their young, unlike honeybees, which collect plant pollen as baby food. Another difference: A honeybee dies after its single-use stinger rips out of its body. Hornets, however, are among the insects that can sting and sting again.
The latest hornet identification key lists 22 species: striped and spangled in various browns and rusts, gold and bluish-blacks. North America also has several native wasps popularly nicknamed hornets. These natives, however, belong on a nearby but different twig of the insect evolutionary tree.
More ‘murder hornets’ are turning up. Here’s what you need to know
Thursday, May 7, 2020
The coronavirus pandemic circling the globe is caused by a natural virus, not one made in a lab, a new study says.
The virus’s genetic makeup reveals that SARS-CoV-2 isn’t a mishmash of known viruses, as might be expected if it were human-made. And it has unusual features that have only recently been identified in scaly anteaters called pangolins, evidence that the virus came from nature, Kristian Andersen and his colleagues report March 17 in Nature Medicine.
When Andersen, an infectious disease researcher at the Scripps Research Institute in La Jolla, Calif., first heard about the coronavirus causing an outbreak in China, he wondered where the virus came from. Initially, researchers thought the virus was being spread by repeated infections jumping from animals in a seafood market in Wuhan, China, into humans and then being passed person to person. Analysis from other researchers has since suggested that the virus probably jumped only once from an animal into a person and has been spread human to human since about mid-November (SN: 3/4/20).
But shortly after the virus’s genetic makeup was revealed in early January, rumors began bubbling up that maybe the virus was engineered in a lab and either intentionally or accidentally released.
An unfortunate coincidence fueled conspiracy theorists, says Robert Garry, a virologist at Tulane University in New Orleans. The Wuhan Institute of Virology is “in very close proximity to” the seafood market, and has conducted research on viruses, including coronaviruses, found in bats that have potential to cause disease in people. “That led people to think that, oh, it escaped and went down the sewers, or somebody walked out of their lab and went over to the market or something,” Garry says.
Accidental releases of viruses, including SARS, have happened from other labs in the past. So “this is not something you can just dismiss out of hand,” Andersen says. “That would be foolish.”
Looking for clues
Andersen assembled a team of evolutionary biologists and virologists, including Garry, from several countries to analyze the virus for clues that it could have been human-made, or grown in and accidentally released from a lab.
“We said, ‘Let’s take this theory — of which there are multiple different versions — that the virus has a non-natural origin … as a serious potential hypothesis,’ ” Andersen says.
Meeting via Slack and other virtual portals, the researchers analyzed the virus’s genetic makeup, or RNA sequence, for clues about its origin.
It was clear “almost overnight” that the virus wasn’t human-made, Andersen says. Anyone hoping to create a virus would need to work with already known viruses and engineer them to have desired properties.
But the SARS-CoV-2 virus has components that differ from those of previously known viruses, so they had to come from an unknown virus or viruses in nature. “Genetic data irrefutably show that SARS-CoV-2 is not derived from any previously used virus backbone,” Andersen and colleagues write in the study.
“This is not a virus somebody would have conceived of and cobbled together. It has too many distinct features, some of which are counterintuitive,” Garry says. “You wouldn’t do this if you were trying to make a more deadly virus.”
No, the coronavirus wasn’t made in a lab. A genetic analysis shows it’s from nature
Thursday, April 23, 2020

Researchers identify cells likely targeted by COVID-19 virus



